Polypharmacy Decoded: 5 Snippets of Nonstop Work and Hidden Effort
While I will dive deeper into the following five areas in future posts, here’s a condensed glimpse into the intricate dance of polypharmacy and the relentless medication work at Northwood (and likely at all other LTCFs). Each of these snapshots reveals how the flow of medications—something that might seem mundane—is, in fact, an unyielding collective enterprise, saturated with stories of effort, unintended consequences, and endurance.
1. Doctor Day, the bi-annual form, and the missing resident
2. The burden of treatment for residents at Northwood
3. Polypharmacy is hard work: solving the medication mystery and handover dilemma
4. How forms shape activities and identities at Northwood
5. Polypharmacy is an organizational practice
My empirical findings demonstrate how medication work or “doing polypharmacy” is accomplished. The work of polypharmacy is relentless and demanding. It is a collective, shared enterprise between the prescribers, residents, other HCPs, medications, and cultural ideas and practices (rules, forms, etc) of what is acceptable at Northwood.
1. Doctor Day, The Bi-Annual Form, and the Missing Resident
In two vignettes, Ativan and Teva, we witness the peculiar yet widely accepted rhythm of Doctor Day, where the nurse and physician orbit the six-month medication review form, a document so vital it dictates the medication flow at Northwood. Within the number-locked nurses’ room, a space where the absent residents are conjured through questions and chart notes, the bi-annual form orchestrates an intricate ritual of knowing. Here, the resident becomes both visible and invisible—a figure reconstructed from fragments of conversation, paperwork, and memory. The physician and the LPN bring the resident to life through their conversations—asking and answering questions, piecing together fragments of information, investigating details, and documenting the absent resident’s story in the charts. The work unfolds in repetitive ways: the physician asks questions and the LPN answers, pens scratching against paper, binders opening and closing, and the urgency to ensure the medications keep flowing.
2. The Burden of Treatment for Northwood Residents
For Northwood’s frail and vulnerable residents, the burden isn’t just their illness—it’s the constant effort to manage the treatments meant to sustain them. These residents are locked in a quiet struggle, caught between the rigidity of institutional care and the messy, embodied reality of living with chronic conditions. One resident confessed, “I line up my pills by shape and color to catch mistakes.” Another voiced their frustration: “I think the doctor decides everything without even seeing me.” This burden of treatment—unseen and unmeasured—demands notice. It calls for a new kind of care, one that prioritizes minimally disruptive medicine, shifting focus from disease to the person enduring its effects.
3. Polypharmacy is Hard Work: Solving the Medication Mystery or Handover Dilemma
In Mrs. J’s Medication Mystery, we see polypharmacy work laid bare: an incomplete hospital form sets off a cascade of repair work spanning hours and multiple organizations. The simple question—“Is she on 26 or 28 medications?”—becomes a sprawling investigation involving nurses, pharmacists, forms, and faxes. The answers are never stable; knowing is a process of reconstruction, a relentless pursuit of fragments scattered across charts, systems, and memories. The work is exhausting, the stakes are high, and yet, the rhythm of polypharmacy demands that it all be done again tomorrow.
4. How Forms Shape Activities and Identities at Northwood
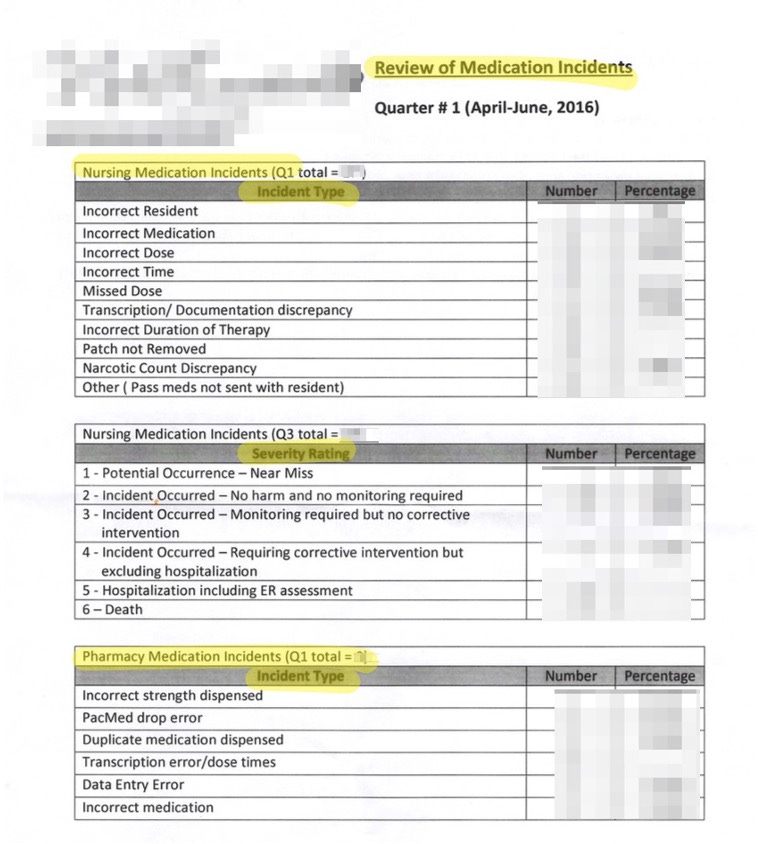
At Northwood, a high accountability institution, forms don’t just record actions; they shape them. Consider the quarterly medication incident review form (the 2026 form below has been replaced in 2019), which categorizes nursing and pharmacy errors but omits prescribing altogether. It’s a subtle exclusion with weighty implications: physicians are untouchable, their actions shielded from feedback loops that others endure. As one nurse put it, “When it comes to physicians, there’s no feedback, no boss.” Forms like these silently reinforce hierarchies, dictate workflows, and even mold the identities of those who use them. They’re not just tools; they’re cultural artifacts, shaping how people think, act, and perceive their place in the system.
5. Polypharmacy is an Organizational Practice
Polypharmacy isn’t a side effect of prescribing, though it is that as well—it’s a living, breathing practice embedded within the institution. It’s an unending cycle of coordination and care, requiring the alignment of people, objects, and routines. From the maroon binders in the nurses’ room to the medication carts rattling down the hall, every element at Northwood is choreographed to keep the flow of drugs uninterrupted. Yet, this practice doesn’t exist without cost. It shapes identities, power dynamics, and the everyday lives of residents and healthcare workers alike. Polypharmacy is not just something Northwood does; it’s something Northwood (and all LTCF’s) is.